Training your calves is a smart move to make — it cuts down on injury risk, improves physical and athletic performance, and adds some shape to your legs. But calf training should never come at the expense of incurring foot pain in the process. So, this article will walk you through what this issue can signify and how to get back to pumping out more calf raises while leaving out the foot pain.
Foot pain with calf raises can arise for multiple reasons. Common reasons include plantar fasciitis, Achilles tendinopathy, tibialis posterior dysfunction, and excessively heavy loading parameters. Solutions involve improving muscle and tendon health and using appropriate training parameters.
So, keep on reading if you want to know who is at the greatest risk of these common conditions, why they arise, and most importantly, how to get these issues under control.

Related article: How to Squat and Deadlift with Plantar Fasciitis: A Complete Guide
As we dive into this article, keep in mind that the foot is a complex region of the body (it has 26 bones and 33 joints, for example). As such, there could be numerous factors for your pain or discomfort. Nonetheless, what follows are some of the most common orthopedic issues that active (and otherwise healthy) individuals incur when training their calves. Use this information to help get you pointed in the general direction for getting to the underlying cause of your pain or discomfort.
As always, getting an assessment from a qualified professional is always a smart move to make if your pain is severe or ongoing. See the disclaimer page for more information.
Issue 1: Plantar fasciitis

Plantar fasciitis is a relatively common condition that causes pain and discomfort on the bottom of the foot. It’s believed to affect around 10% of the global population at one point in an individual’s life.1
At its heart, plantar fasciitis is a degenerative condition affecting the plantar fascia. The plantar fascia is a thick, fibrous band of connective tissue on the bottom of the foot, which runs from the heel out to the midfoot and toes. While the pain can be felt anywhere on the bottom of the foot, it is most often experienced right around the bottom of the heel. Take a look at the pain map below for a visualization.
Pro tip: The scientific community is starting to fall out of favour with the term “plantar fasciitis” because the name is a bit of a misnomer. (The suffix “itis” refers to a process of inflammation taking place within the tissue; however, there typically isn’t much inflammation involved with plantar “fasciitis.”)2–4
Causes of plantar fasciitis
There are numerous reasons why plantar fasciitis can occur. Some of the most common causes include (but are not limited to):
- Poor biomechanics of the foot and ankle, which can include poor ankle mobility and arch issues (such as being flat-footed, otherwise known as pes planus).2
- A high body mass index (BMI), which is typically seen in those with a BMI above 30.5
- Tightness or weakness of the muscles and tendons on the back of the lower leg (the gastrocnemius muscle, the soleus muscle, and the Achilles tendon).2
- A high volume of high-impact or weight-bearing activities such as running and walking.2
Treating plantar fasciitis
Thankfully, while often stubborn, plantar fasciitis tends to have good outcomes with conservative treatment. Upwards of 90% of individuals affected with this condition respond to conservative measures.5 Depending on the severity and chronicity (how long the issue has been going on), it may take weeks or even months to fully resolve; however, the outcomes are usually rather favorable.
Related article: Plantar Fasciitis Taping: A MUCH More Effective Way (All By Yourself!)
Conservative measures that are typically helpful can include:
- Correcting the biomechanics of the foot and ankle, such as improving ankle joint mobility.
- Taping techniques, such as the Low Dye technique to reduce pain.
- Extracorporeal shockwave therapy (ESWT), which has been found in numerous studies to be beneficial in reducing the symptoms of plantar fasciitis
- Stretching the muscles and tissues of the foot, ankle, and lower leg that may be otherwise chronically tight.
Fun story: I once treated a semi-pro baseball catcher who couldn’t squat down into his stance due to the pain he was having in his plantar fascia. I performed one treatment session only on his calves (due to my clinical reasoning) without even touching his plantar fascia. When I followed up with him a few months later, he said he hadn’t had a single bout of heel pain after that one treatment. Crazy stuff, eh?
Issue 2: Achilles tendinopathy
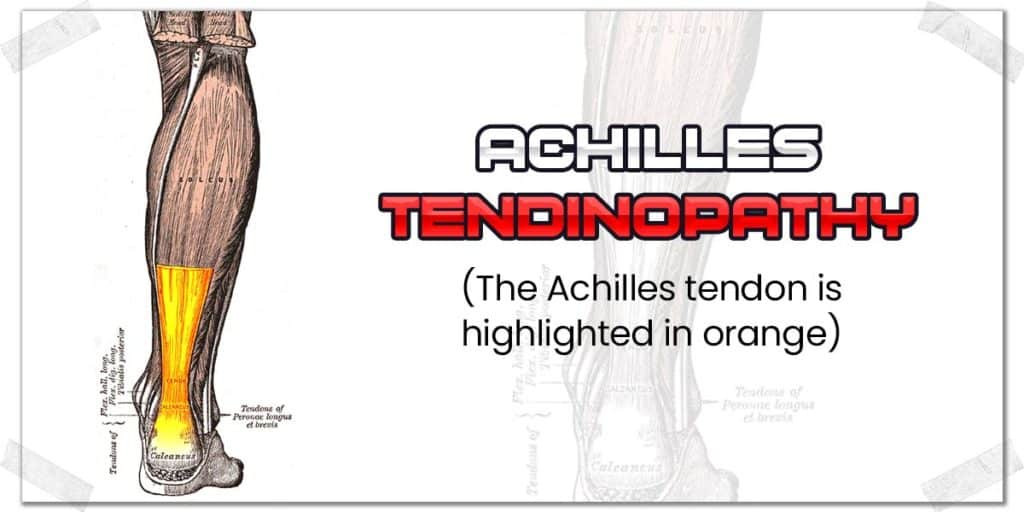
The Achilles tendon is the thick cord-like structure you can see and feel just above your heel on the back of your leg. Its purpose is to transmit the contractile force from the muscles on the backside of the lower leg (the gastrocnemius and soleus muscles) down to the heel bone, where it attaches. When the muscles contract, the Achilles tendon pulls on the heel, causing the ankle to point the foot downward (known as plantarflexion).
The Achilles tendon can become unhealthy and painful for numerous reasons. Since it is a tendon, the generalized term for an unhealthy tendon is tendinopathy, hence the term Achilles tendinopathy.
The Achilles tendon can become unhealthy in different ways, and while the specifics are beyond the scope of this article, the most common forms of tendinopathy for this tendon include:
- Achilles tendinosis
- Achilles tendonitis
- Achilles tenosynovitis.
The tendon itself can become unhealthy anywhere within the tendon, including the musculotendinous junction, the mid-portion of the tendon, or near its insertion point onto the calcaneus (heel bone).
Pro tip: The actual condition of tendinitis isn’t nearly as common as we used to once believe it to be. Most often, tendons that are overused and sore display characteristics of tendinosis. (The suffix “itis” refers to a process of active inflammation within the tendon). This inflammation is typically short-lived within the tendon. Hence, tendinosis is more commonly found in unhealthy tendons.6
Causes of Achilles Tendinosis
The Achilles tendon can become unhealthy either due to excessive movement and strain (overuse) or from a lack of adequate movement (underuse). It is believed that the most common reason for Achilles tendinosis to arise is due to excessive loading (stressing) of the tendon with inadequate periods of rest and recovery.
Additional factors that can also predispose the Achilles tendon to become unhealthy include stiffness or loss of pliability to the tendon, poor biomechanics (movement mechanics) when walking or running, and poor muscle health of the gastrocnemius (calf) and soleus muscles, to which both attach to the Achilles tendon.
As with any other condition, determining the underlying cause is the cornerstone to effective recovery; if you don’t fix the underlying mechanism that’s creating the issue, it’s very likely that it will return at a later time.
More concisely put: treat causes, not symptoms.
Treating Achilles Tendinosis

Rehabbing the Achilles’ tendon back to full health can be a time-consuming process, depending on how unhealthy the tendon is and for how long it’s been in such a condition. Still, just as with plantar fasciitis, conservative measures tend to produce quite favorable results when the respective parameters are dialled in appropriately.
As a general rule, tendons don’t get healthier with only rest (they might feel better when you rest them, but the pain will return when you attempt to resume your physical activities). However, they can become overloaded and painful with too many activities. Essentially, it’s a delicate balance between stimulating them appropriately but not overloading them in the process.
Some scientifically established conservative interventions that can be profoundly helpful for rehabbing an unhealthy Achilles tendon include:
- The Alfredson’s heal drop protocol6,7
- Extracorporeal shockwave therapy6,7
- Utilizing a heel cushion or heel cup within your shoe6,7
- Correcting biomechanical issues within the foot6,7
- Taping or bracing interventions6,7
Generally speaking, a combination of multiple interventions will likely yield the most optimal outcome, as multiple interventions can help to produce synergistic effects for tendon health.
Tendon loading is the cornerstone to effective tendon rehabilitation, so ultimately, you’ll want to find ways to stimulate and strengthen the tendon appropriately. The ideal ways to do so can be highly variable, depending on numerous factors. If you’d like to read up on some of the details, you can check out these scientific articles for starters:
Article 1: Pathophysiology and nonoperative treatment (National Library of Medicine)
Issue 3: Tibialis posterior issues

The tibialis posterior muscle is a much lesser known muscle (and tendon) than the Achilles tendon; however, it can become unhealthy (and painful) through the exact same means and for the same reasons as the Achilles tendon.
The tibialis posterior is a deep muscle of the lower leg that turns into a long tendon that runs all the way down to the underside of the foot. The muscle works to help produce plantarflexion of the ankle (i.e., the exact same movement as when performing calf raises).
Anatomy tip: The tibialis posterior tendon plays a key role in forming and stabilizing one of the prominent inner arches of the foot (known as the inner longitudinal arch).
Dysfunction of the tibialis posterior muscle or tendon can lead to:
- Pain or discomfort in the mid-calf region underneath the calf muscles
- Loss or collapse of this foot arch
- Pain or discomfort experienced along the inside portion of the ankle
- Pain or discomfort on the bottom (sole) of the foot

Pro tip: In addition to the tibialis posterior muscle, two other tendons sit next door to this muscle. They are the flexor hallucis longus and the flexor digitorum longus. While either of these tendons can also become unhealthy, in my clinical experience, the tibialis posterior muscle is by far the most commonly involved muscle of the three that leads to foot pain.
Causes of tibialis posterior tendinopathy
While there can be numerous reasons for dysfunction and breakdown within the tibialis posterior tendon, some of the more common causes are poor ankle and foot biomechanics and repetitive, impact-based activities.8 Let’s look at these in a bit more detail. From there, I’ll present information on how to treat the issue.
Poor ankle and foot biomechanics

The biomechanics of the foot can play a prominent role in one of the reasons for the tibialis posterior tendon to become unhealthy, which can lead to a condition known as posterior tibial tendon dysfunction. When the forefoot rolls inwards (known as pronation) or there is excessive eversion of the calcaneus (heel bone), excessive stress and strain can be placed on the tendon, which can cause it to weaken or become irritated. Sometimes this can become severe enough to cause a loss or total collapse of the arch of the foot.
Related article: Four Handy Exercises to Help Loosen Stiff Ankles in All Directions
If such poor biomechanics are already present, and calf raises are then being performed, in some individuals, it can create excessively high levels of stress and strain on the tendon (especially if performing calf raises one leg at a time or with high levels of resistance, such as using a calf raise machine), which can lead to acute (newly occurring) or chronic (persistent and ongoing) irritation and pain arising from the tendon.
Repetitive impact-based activities
Additionally, performing highly repetitive activities that involve impactful forces to the bottom of the foot (jogging, running, rope skipping, jumping, etc.) have been shown to be relatively common causes of pain and dysfunction within the tibialis posterior tendon.
As such, if you’ve been performing heavy calf raises (which can stress the tibialis posterior tendon) or frequent and repetitive, impact-based activities, it’s possible that the poor tendon has been taking a beating to the point of now becoming overworked and painful.
If you feel this to be the case, it may be worth re-evaluating your training routines and finding ways to cut back on the load and stresses of what the bottom of your foot is enduring.
Treating tibialis posterior tendinopathy
Treating tibialis posterior tendinopathy requires much of the same approach as with Achilles tendinopathy (or any tendinopathy, for that matter). As a result, read through the section above on treating Achilles tendinopathy, as much of that information pertains to how to effectively treat the tibialis posterior tendon as well.
However, there are a few unique features to be aware of with this tendon, so let’s quickly go over those.
Conservative measures that are typically helpful can include:
- Correcting the biomechanics of the foot and ankle, which can include strengthening the intrinsic muscles of the foot.
- Low Dye taping to help structurally offload and support the inner arch of the foot (note this is a helpful adjunct but not necessarily a cure).
- Treating the belly of the tibialis posterior muscle (if it’s found to be tight and painful). It’s a tricky muscle to access but can be treated with interventions such as intramuscular stimulation (IMS).
- Strengthening the tibialis posterior muscle if it’s found to be weak or underactive.
Again, every individual’s case is unique, and it often takes a combination of interventions (and different durations of time) to optimize muscle and tendon recovery.
Issue 4: Excessive training parameters
As robust and vigorous as feet can be, they aren’t bulletproof. And in the absence of sudden trauma (rolling your ankle, stubbing your toe, etc.), the ankle’s tissues and structures can become sore through overuse, poor mechanics, or some combination of the two. (Remember, this is a common reason for tendinopathy to occur in the Achilles and tibialis posterior tendons).
Stimulating tendons through resistance exercise is very important for overall orthopedic health. However, overstimulation will lead to the tendons, muscles and other associated tissues becoming sore, painful, or otherwise unhealthy if this resistance is excessive or highly repetitive in nature without adequate time to recover in between activities or training sessions.
Even if you’re only performing calf raises or similar strengthening exercises a couple of times per week but are performing additional activities such as running, sprinting, stair running, etc., such activities can contribute to the accumulating overload of the muscles, tendons, joints, and other structures of the foot and ankle.
As a result, you’d be wise to have alternative forms of exercise to implement if your foot or ankle (or feet and ankles) are acting up. Pushing through pain will only get you so far. Examples could include switching from running to the rowing machine or elliptical machine, which will take out the repetitive landing forces placed through the foot when running. You could also opt to perform swimming, if practical to do so.
Pro tip: Get in the mindset of training to stimulate, not annihilate, your muscles, joints and tendons.
Here are some highly effective tips to keep in mind for ensuring you’re not doing more harm than good when training your calves:
- Training = stress + rest. Do not neglect the rest portion of this equation.
- Read up on the concept of minimal effective training dose to learn how to ensure you’re adequately stimulating your muscles and tendons without running the risk of overdoing things.
- Don’t neglect your recovery. The harder and more frequently you train, the harder and more frequently you should perform recovery-based interventions.
Related article: The Seven Best Ways to Massage Your Calf Muscles All By Yourself
How often to train your calves
While people have different reasons and different ways for training their calves, there are some general rules to keep in mind, regardless of the why or how for your training.
- The more frequent your training sessions for your calves, the less intensity you should consider using. If you train them every other day, the intensity and volume will need to be much lower than if you were to only train them once or twice per week.
- For general strength training, two or three training sessions per week should be all that it takes, provided you’re training the muscles with either high volume or high intensity.
Bonus: Lesser known issues

As with any other blog article discussing pain and dysfunction, I can’t cover everything within a single post, so I tend to stick with the most common issues, as common things are, well…common.
Nonetheless, some less common issues can cause foot pain when performing calf raises or other such exercises. What follows are some brief descriptions of other conditions that, while not as common, certainly aren’t unheard of, either. For your convenience, I’ll provide links for further reading to each one.
The descriptions I provide are merely to help point you in the right direction for further exploration of the potential mechanism(s) causing or contributing to your issue.
Cuboid syndrome
The cuboid is a small bone on the outside edge of the foot. For numerous (and often poorly understood) reasons, the joint function between the cuboid and the calcaneus (the heel bone) can become disrupted, which can lead to various symptoms of discomfort or pain in the foot. It tends to occur after a sudden or traumatic injury to the foot, such as rolling and spraining the ankle.
For more information, you can check out this physio-pedia article on cuboid syndrome.
Lisfranc fracture
As with cuboid syndrome, a Lisfranc injury tends to most often occur from a sudden, forceful (and traumatic) injury to the midfoot region. As a result, it shouldn’t be suspected if you haven’t recently had any traumatic injury to your foot or ankle.
Nonetheless, it can be a source of pain to those who have unknowingly previously received this injury without proper diagnosis. The injury results in a disruption of the tarsal and metatarsal bones in the midfoot, and as such, tends to produce pain in the midfoot region.
For more information, you can check out this physio-pedia article on Lisfranc injuries.
Morton’s neuroma
Morton’s neuroma is a condition involving the entrapment of one or more of the plantar digital nerves of the foot. It can result in altered sensations and pain around the midfoot region or the metatarsals. The hallmark sign of this condition is the location of discomfort or pain along with the type of sensations that are felt.
To learn more, check out this physio-pedia article on Morton’s Neuroma:
Hallux valgus
Hallux valgus, otherwise known as a bunion, is the resulting deformity of the big toe in relation to the rest of the foot. The condition involves the alteration of the metatarsophalangeal (MTP) joint of the first toe so that it begins to point outwards (away from the body’s midline) instead of staying aligned straight ahead.
It’s not fully understood why bunions often occur; however it is well known that they can lead to pain and disability within the foot. They aren’t always painful, and as such, if you don’t have any signs of bunion formation on your foot, there’s no reason to suspect this to be the source of your foot pain.
To learn more, check out this physio-pedia article on Hallux valgus
Arthritis of the great toe (Hallux rigidus)
Hallux rigidus a degenerative condition involving the breakdown of the first metatarsophalangeal (MTP) joint of the foot (i.e., the big toe). It leads to stiffening (loss of range of motion) throughout the joint due to the arthritic changes taking place within the joint. The result can be pain experienced with activities such as walking, calf raises, or any other activity involving lifting the heel off the ground while keeping the toes grounded (which produces extension of the MTP joint). The pain is most often experienced around the base of the big toe, where the joint is.
To learn more, check out this physio-pedia article on Hallux rididus
Final thoughts
There can be many reasons why you’re experiencing foot pain when doing calf exercises; remember, the foot and ankle is a highly complex region of the body. It’s not uncommon for aches and pains to occur in the feet from time to time. If, however, it’s occurring every time you work your calves, you’ll want to do a deeper dive into the reasons as to why this may be.
Take the time to seek appropriate guidance and treatment for your pain. Doing so may be annoying, but it will help to optimize the recovery process and minimize the time it takes to get back to pain-free training.
Happy lifting!
References:
5. Plantar Fasciitis. Physiopedia. Accessed August 4, 2022. https://www.physio-pedia.com/Plantar_Fasciitis
8. Posterior Tibial Tendon Dysfunction. Physiopedia. Accessed August 4, 2022. https://www.physio-pedia.com/Posterior_Tibial_Tendon_Dysfunction

Hi! I’m Jim Wittstrom, PT, DPT, CSCS, Pn1.
I am a physical therapist who is passionate about all things pertaining to strength & conditioning, human movement, injury prevention and rehabilitation. I created StrengthResurgence.com in order to help others become stronger and healthier. I also love helping aspiring students and therapists fulfill their dreams of becoming successful in school and within their clinical PT practice. Thanks for checking out my site!

