If you’re in the market for finding and delivering an in-service topic as part of your PT student requirements, this article will hopefully help you out.
This article covers ten topics that could make for great presentations in order to satisfy your in-service requirements.
And, if you haven’t already done so, be sure to check out my other in-service articles:
• The BEST PT Student In-service Topics of 2022 | Check THESE Out
• In-service Presentation & Topic Ideas for PT Students: Ten Great Ideas
Article overview (Quick links)
Click/tap on any of the following topics to instantly jump to that particular topic.
- EMDR therapy for phantom limb pain
- The PoNS Neurostimulator
- The Shoulder Sphere for treatment of rotator cuff issues
- The beehive theory in traumatic brain injury/concussion/CTE
- P-DTR for the treatment of neuromuscular pain
- The SFMA for clinical evaluation of orthopedic conditions
- EOS imaging (3D X-rays)
- The MoBo board
- Cloward point referrals for the implication of cervical disc issues
- eToims treatment for neuromuscular-based injuries
Topic 1: EMDR therapy for the treatment of phantom limb pain
Most ideal clinical setting: Neuro, general outpatient, chronic pain
Great paper to read: EMDR as a treatment for phantom limb pain
Another great paper to read: Treatment of chronic phantom limb pain using a trauma-based psychological approach
What it is: EMDR (Eye Movement Desensitization and Reprocessing) is a form of psychotherapy that is often used for the treatment of psychologically troublesome or disturbing memories, such as for those dealing with symptoms of PTSD. I’ve been casually studying it for the past year or so. The general premise behind it is through the use of bilateral stimulation (most often visual, but can also be auditory or movement-based as well).
While performing EMDR for the treatment of psychological issues is clearly out of the scope of the physical therapist, there is some very neat evidence that shows the effects that EMDR can have for pain reduction, specifically for those dealing with phantom limb pain.
While I have particular ideas as to the specific mechanisms behind its physically pain-relieving phenomenon (my various theories are beyond the scope of this article), I have seen it first-hand within my clinic; having my patients perform lateral eye movements (not for treating psychological issues) have dramatically knocked down dural whole-body tension in many of my patients when they present with global dural tension.
Sounds like hocus pocus-type stuff, I know. But there is clearly a link between bilateral stimulation within the hemispheres of the brain and pain reduction for specific types of pain, particularly pain associated with midline crossing issues.
Why it could be a valuable in-service presentation
The evidence behind EMDR as an effective treatment for certain psychological issues is fairly established and continues to mount. As a result, there is some emerging research taking place on its effects on sensorimotor deficits and body image-related pain. Since sensorimotor disturbances can lead to peculiar types of pain presentations, the implementation of bilateral stimulation as a means to clean up some of the pain that comes with these disturbances is in fact quite an exciting topic to study (I’m currently reading up on it as much as I can since I find it downright fascinating).
After all, he who fully understands how to treat chronic pain and body image-based pain holds the keys to the universe.
Topic 2: The PoNS Neurostimulator for gait & balance rehab
Most ideal clinical setting: Neuro, geriatrics
Website: https://www.ponstreatment.ca/en/
What it is: The PonNS (Portable Neuromodulation Stimulator) is billed as an innovative medical device that can be used for conditions such as traumatic brain injury (TBI) and multiple sclerosis (MS). The device works by providing gentle electrical stimulation to the tongue, which then stimulates the brainstem. The belief is that this form of stimulation can help with enabling neuroplasticity within the brain, which can be therapeutic and beneficial to patients in a myriad of ways.
I will be the first to admit that neuro rehab is not my strong suit, however, I’ve looked into the PoNS enough to indeed become intrigued by it as well as the potential benefits that it may have for those with certain neurological issues.
Why it could be a valuable in-service presentation
According to their website, the PoNS device can be used for various aspects of rehab, such as balance training and gait training. It likely has other potential uses as well, however, I’m simply not overly familiar with the PoNS at this point in time. Nonetheless, a neuro-rehab device that could help with balance and/or gait retraining could be well worth learning more about. Informing other clinicians of the existence of this device and its purported therapeutic and rehabilitative benefits could make for a great and enlightening in-service presentation.
Topic 3: The Shoulder Sphere for the treatment and rehab of rotator cuff pathologies
Most ideal clinical setting: Orthopedics, general outpatient
Website: https://www.shouldersphere.com/
What it is: The Shoulder Sphere is the brainchild of Dr. Win Chang, an M.D. who is a former Clinical Assistant Professor of Orthopedic Surgery at New York University Hospital for Joint Diseases. He specialized in orthopedic surgeries for shoulders, elbows, hips and knees. Rotator cuff surgery was one of his specialties.
In short, the Shoulder Sphere is a patented rotator cuff strengthening device that strengthens the rotator cuff muscles in a multidirectional manner. It’s used by many an athlete around the world, ranging from amateur to professional. You can think of it as a more modern (and perhaps more dynamic) version of a shoulder/rotator cuff device such as the body blade.
Why it could be a valuable in-service presentation
Live long enough and you’ll experience a rotator cuff issue of some sort. Since approximately 25% of the population above the age of 60 are said to have at least one partial rotator cuff tear, it’s a good idea to be well informed on various rotator cuff strengthening protocols along with different rehabilitative devices. Rotator cuff issues are going to be one of the more common issues you’ll evaluate and treat if you plan on working in an orthopedic or general-practice outpatient-based setting.
Not only will your knowledge of rotator cuff rehab devices help your patients get better treatment and outcomes, but it will simultaneously make you look like a rockstar in the process.
As well, the Shoulder Sphere website is chock-full of all sorts of information pertaining to their device, so it should be pretty darn easy to put together a presentation based on all of the information on their site!
Topic 4: The beehive theory in traumatic brain injury/concussion/CTE
Most ideal clinical setting: Any
Great paper to read: The Beehive Theory: Role of microorganisms in late sequale of traumatic brain injury and chronic traumatic encephalopathy
What it is: Just as if you were to experience a swarm of bees fleeing a tranquil beehive if you were to disturb their hive, the beehive theory in traumatic brain injury postulates that a blow to the head can disrupt and release various microorganisms and microbiota in the brain and throughout the body. This disturbance can wreak havoc on the body and subsequent healing process required, just as a swarm of agitated bees who have had their hive disturbed can wreak havoc on nearby humans.
Why it could be a valuable in-service presentation
Concussion management and treatment is a pretty hot topic in the world of physical therapy and rehabilitation-based practices these days. There are still tons we don’t know about concussions and subsequent rehabilitation from them, however, the beehive theory is really unique in that it takes a look at the systemic changes that can occur throughout the body as the result of any form of TBI.
These adverse systemic changes could in fact be overlooked key aspects when it comes to effective and optimized TBI rehabilitation. Guaranteed that no matter how much your CI’s or other clinicians may know about concussion rehab, there is still plenty for them (and everyone else) to continually learn. No one knows everything, and for those who want to take a broader-based theoretical look at TBI/concussion rehab, the beehive theory is a great theory to read up on and present as an in-service topic.
Topic 5: P-DTR for the treatment of neuromuscular pain
Most ideal clinical setting: Orthopedics, general outpatient, neuro
Website: pdtr-global.com/
What it is: Proprioceptive Deep Tendon Reflex (P-DTR) is the product of orthopedic surgeon Dr. Jose Palomar. It is a treatment system based on various systems of the body, including neurology, neurophysiology and biomechanics.
It is a system that relies heavily on the brain’s perception and interpretation of various sensory stimuli in the formation of pain. P-DTR examines the different types of sensory input signals that the brain receives and aims at identifying if they are causing or contributing to the individual’s pain.
What I really like about this system is their analogy in thinking of the body as a struggling computer system; P-DTR classifies pain into “hardware” based problems and “software” based problems. A hardware problem would be a physical issue (tendinopathic tissue breakdown, osteochondrosis, etc.) within the body while a software issue could be thought of as little glitches in the programming and operation of the computer. It’s the detection of these “software” pain-based presentations that P-DTR is designed to identify and treat.
Why it could be a valuable in-service presentation
Physical therapists are often trained in looking at issues within the body as “hardware”-based issues. Much of the time this is indeed what we deal with, however, there are plenty of times in which pain and perceptions of pain are arising from nervous systems-based issues. I know that for me, personally, I didn’t receive much training on this while in school, which is unfortunate since the world of pain science is continually showing us that “software” issues commonly drive or at least contribute to the pain of those who end up in physical therapy clinics.
Providing an in-service on a system such as P-DTR, which aims to identify, treat and resolve sensory-based pain issues could be enlightening for those whom you’re presenting to. I personally know a few P-DTR practitioners and I’ve seen them have some amazing treatment sessions and outcomes on their patients.
Topic 6: The SFMA for clinical evaluation of orthopedic conditions
Most ideal clinical setting: General outpatient
Website: https://www.functionalmovement.com/
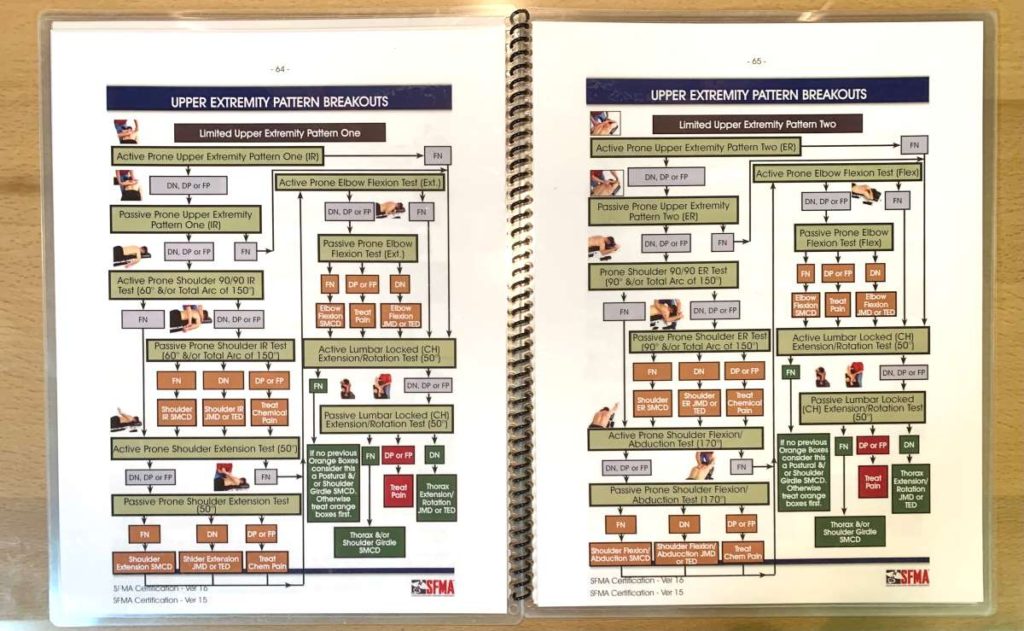
What it is: The SFMA (Selective Functional Movement Analysis) is a systematic evaluation-based protocol for taking a deeper look at determining the primary causes for a patient’s musculoskeletal pain. It is the product of Functional Movement Systems and the brainchild of Gray Cook and Gary Gray. It is the “big brother” version of Functional Movement’s Functional Movement Screen (FMS).
Related: The Functional Movement Screen: Why New PT Grads Should Know it
The SFMA is compromised of a series of general movements that the patient performs. Based on the outcome of each respective movement, further movements specific to each one of the general movements are then performed.
These specific movements are known as “breakouts” and help the clinician to determine the exact cause of pain/dysfunction categorize it as either a mobility issue, a joint stability issue or a motor control issue. It is through these breakouts and classification of each respective outcome that allow the physical therapist to determine the root cause of movement dysfunction, be it painful or non-painful.
Why it could be a valuable in-service presentation
Having a systematic approach during patient evaluations can be incredibly beneficial for the practitioner. Being able to classify movement disorders into particular categories along with having strategies for how to best correct each one can help to identify the root cause of a movement issue much more quickly and accurately while also ensuring better outcomes for the patient.
The SFMA is a pretty well-known and often implemented system in the world of orthopedic physical therapy, so shining some light on this system to clinicians who may not be aware of its widespread use and its subsequent efficacy could make for a great presentation topic.
Topic 7: EOS imaging (3D X-rays)
Most ideal clinical setting: Orthopedics
Website: https://www.eos-imaging.com/
What it is: EOS imaging is a remarkable new form of X-ray technology, offering super low dose radiation when compared to traditional plain-film X-rays. What’s even more remarkable is that this technology provides three-dimensional imaging of an individual’s bones/skeletal system.
It’s not primarily used in the traditional sense of looking for broken bones or other diagnostic-based examinations. Rather, it’s more so used for better understanding of an individual’s overall anatomical situation, such as for complex conditions such as scoliosis, surgical planning and much more.
Since it’s a super low dose system, it’s ideal for patients with complex and changing/dynamic skeletal conditions who must undergo more frequent X-ray imaging.
The full-body X-rays are taken in a standing position with one X-ray taken from the front while the other is taken from the side. This allows for a three-dimensional rendering of the individual’s skeletal system, which can reveal much more bone-based information than a standard two-dimensional X-ray.
Why it could be a valuable in-service presentation
It may not seem like something that a physical therapist would directly be involved in, but having an understanding of this technology, its use and its potential impacts on advancing the world of musculoskeletal rehab is pretty critical. It is (in my humble opinion) going to become much more prominent technology that PT’s will be involved with down the road in the not-so-distant future.
Many physical therapists work closely or even directly with orthopedic surgeons and radiologists, so knowing all about the potential impacts of this technology in the world of physical rehabilitation isn’t a bad idea as you move forward into your career.
Not many physical therapists are overly aware of this promising and exciting new technology as of yet, and they’re likely going to need to know all about it if they plan on working for a good length of time into the future. So, if you do your in-service on this topic, not only are they likely to find it interesting but you’ll also look pretty on top of things when it comes to upcoming technology that PT’s are likely going to become aware of in the future.
Topic 8: The MOBO board
Most ideal clinical setting: Orthopedics, general outpatient
Website: https://www.moboboard.com/

What it is: The MOBO board may look like just another balance board, but it’s actually a nifty piece of equipment that can be used for various reasons. I first became introduced to it at our clinic last year and have had fun playing around with it ever since.
The defining feature when looking at it is that there’s no place to rest your toes when standing on the board. When using the board for strengthening-based purposes, the result is an increased demand on the inner longitudinal arch, forcing the patient/individual to stabilize through their first ray.
When using the board, you have the ability to determine the planes of movement you wish to challenge. This is done by simply taking the two bottom rockers and placing them in one of two different orientations underneath the board’s surface.
When using the board for mobility-based purposes, the orientation of motion produced by the board forces the subtalar joint to move in ways that can help with mobilization. Since the subtalar joint is in fact a tri-planar joint, it can be mobilized in varying directions. Not a bad variety of clinical applications for one simple but unique balance board.
Why it could be a valuable in-service presentation
Many patients can benefit from balance and ankle-based training. The MOBO board offers some unique ways to challenge foot intrinsics and mobility that standard balance boards can’t.
It can be a great addition to clinics since its cost is relatively low while also taking up practically no space within the clinic environment. Additionally, it can serve a wide variety of clinical populations and doesn’t take extensive or highly advanced training in order to safely and successfully implement on patients. If your CI or clinic takes a heavy interest in treating foot and/or ankle-based issues, this just might be the perfect in-service topic!
Topic 9: Cloward point referrals for the implication of cervical disc issues
Most ideal clinical setting: Orthopedics, general outpatient
What it is: In the 1950s, before the advent of MRI technology, physicians who wanted to have visual confirmation of disc protrusions within the spine only had one real way to do so: they would take a radioactive compound and would inject it into the disc that they suspected to be bulged or herniated. They would then take X-rays, which would show where the radioactive compound migrated to within the disc – showing a presence or absence of a disc bulge/herniation. Thankfully, we now have MRI technology.
When these injections took place, it soon became very evident that when the freezing compound would wear off that people would complain of very specific areas of pain between or around the shoulder blades, based on which disc had been injected (and thus irritated). Certain disc levels had very strong correlations with the intrascapular areas in which the referral pain was felt. Note: cervical disc referral patterns are not the same thing as cervical zygophophesyal (facet joint) referral patterns.
Why it could be a valuable in-service presentation
I was never briefed or trained on Cloward points during my days of PT school. While obviously not every orthopedic issue can be covered while in school, I feel that this was one that certainly should have; many patients come into PT clinics complaining of intrascapular pain. Unfortunately, many PT’s don’t appreciate or pick up on the potential for this to be a referral point from the cervical discs.
I can’t tell you how many times so far in my young career I’ve seen patients present with intrascapular pain that was actually referral pain from a cervical disc. I’ve had plenty of people come to me after having their shoulder-blade region extensively treated by others, with no relief of symptoms (because, in fact, the pain wasn’t coming from the shoulders or thoracic spine). Makes me look like a rockstar when I then evaluate and treat their neck and get them feeling better.
The awareness of Cloward point referral patterns is critical for appropriate treatment of those complaining of intrascapular-region pain.
Topic 10: eToims treatment for neuromuscular-based injuries
Most ideal clinical setting: General outpatient, orthopedics
Website: https://etoims.com/

What it is: eToims (Electrical Twitch Obtaining Intramuscular Stimulation) therapy is the brainchild of Dr. Jennifer Chu, M.D. I first became introduced to eToims when signing on to work with my current employer, Tower Physiotherapy and Sports Medicine, here in Calgary. We use eToims for various conditions with our patients, based on their individual needs. It’s been pretty cool to see the therapeutic effects that it has provided on many of our patients.
eToims designates itself as a treatment modality that offers the ability to precisely target and stimulate neuromuscular junctions that have been injured, evoking twitch responses in deep tissues not achievable with traditional neuromuscular stimulation. Its unique design allows for quick detection of irritable or injured trigger points, indicating a diagnostic presence of acute or chronic nerve irritation.
Why it could be a valuable in-service presentation
Various forms of electrotherapy, such as the more traditional electrical neuromuscular stimulation (NMES) are widely used in the rehabilitative world for physical therapy. eToims offers a rather different style of approach when attempting to stimulate peripheral nerves and their respective muscles.
On one hand, it affords the clinician a diagnostic approach in the identification of latent trigger points while also offering the ability to serve as a therapeutic treatment intervention. Since eToims markets itself as a modality that can help treat chronic pain due to conditions such as spinal arthrosis, gathering some information on this modality and giving an in-service to others regarding its uses could indeed make for a great presentation.
Concluding remarks
There’s no shortage of potentially amazing clinical in-service topics to present on; the ten ideas listed off in this article are nothing more than the tip of the iceberg. Hopefully, these topics have helped enlighten you to some potential topics you could choose, or have sparked some other ideas and avenues to explore.
Just remember to pick a topic that you’re truly interested in – it will make for a much more enjoyable experience when putting your presentation together and likely a much more enjoyable presentation for your audience.

Hi! I’m Jim Wittstrom, PT, DPT, CSCS, Pn1.
I am a physical therapist who is passionate about all things pertaining to strength & conditioning, human movement, injury prevention and rehabilitation. I created StrengthResurgence.com in order to help others become stronger and healthier. I also love helping aspiring students and therapists fulfill their dreams of becoming successful in school and within their clinical PT practice. Thanks for checking out my site!